Skin – First line of defense
Questions
Common Model Answer (2 Marks)
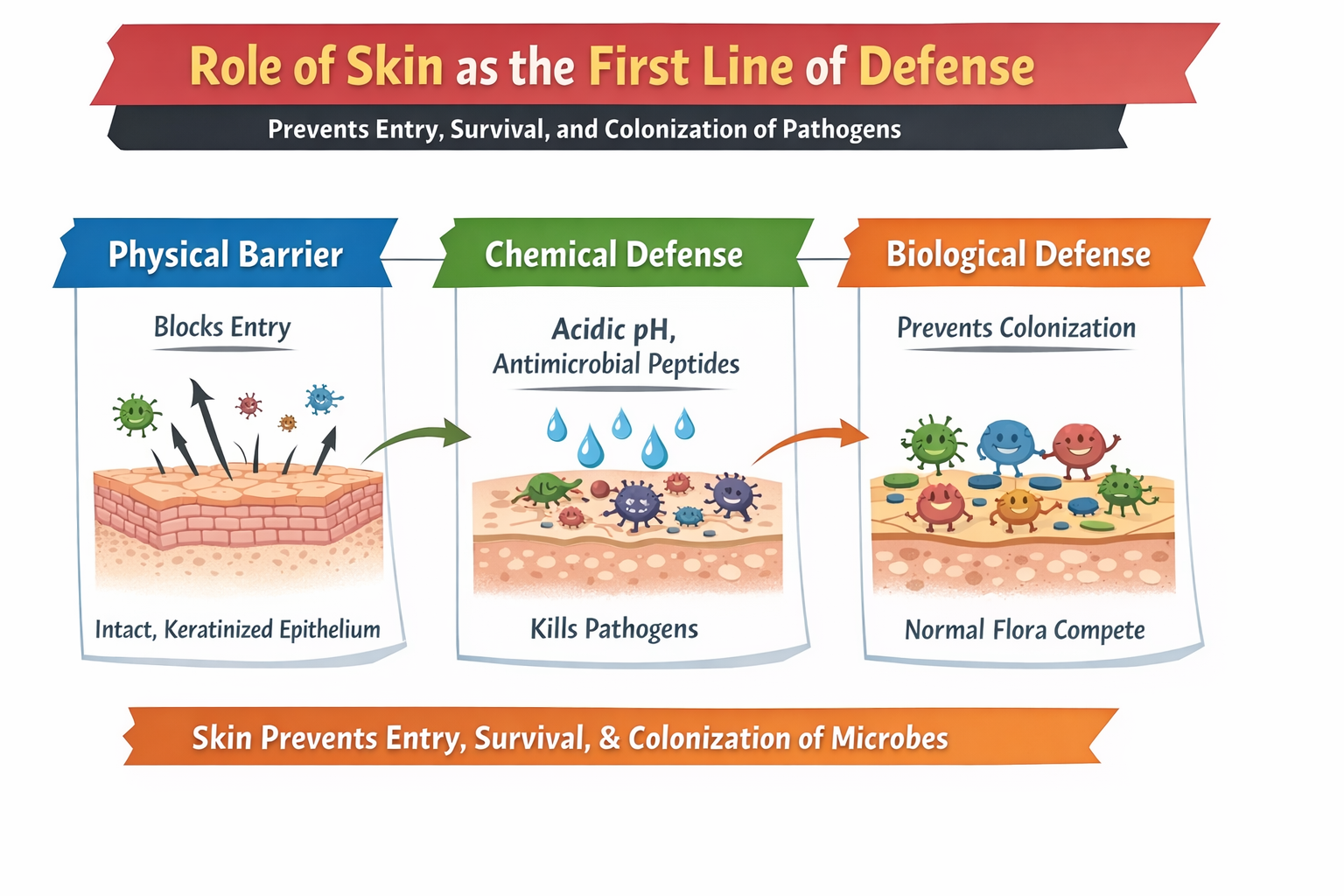
The skin provides innate, non-specific immunity by acting as a physical, chemical, and biological barrier.
- Physical barrier: The keratinized stratified squamous epithelium (stratum corneum) prevents pathogen entry, and desquamation removes attached microbes.
- Chemical & biological barrier: Sebum and sweat maintain an acidic pH (~5.5) and contain lysozyme and defensins, while normal skin flora competes with pathogens and produces bacteriocins, preventing colonization.
Questions
Common Model Answer (4-6 Marks)
The skin forms an essential component of the innate (non-specific) immune system and acts as the first line of defense by preventing the entry, survival, and colonization of pathogens through physical, chemical, and biological mechanisms.
1. Physical (Mechanical) BarrierThe skin consists of a keratinized stratified squamous epithelium, with the outermost stratum corneum composed of dead, keratin-rich cells. This tough, impermeable layer, along with tight intercellular junctions, prevents microbial penetration. Continuous desquamation (shedding) of surface cells mechanically removes adherent microorganisms.
2. Chemical BarrierSkin secretions create a hostile chemical environment for microbes.
- Acidic pH (~5.5): Maintained by sebum (fatty acids secreted by sebaceous glands) and sweat (containing lactic acid), which inhibits bacterial growth.
- Antimicrobial substances: Sweat contains lysozyme, which hydrolyzes bacterial peptidoglycan cell walls. Keratinocytes secrete antimicrobial peptides such as defensins and cathelicidins, which disrupt microbial membranes and kill pathogens.
The skin is colonized by normal commensal flora, which protects against pathogenic organisms through competitive exclusion. These microbes compete for nutrients and attachment sites and produce bacteriocins, which inhibit or destroy competing pathogens, thereby preventing colonization.
Conclusion: Thus, the skin integrates physical, chemical, and biological defenses to block pathogen entry, impair microbial survival, and prevent colonization, making it an effective first line of innate immune defense.
Questions
Common Model Answer (8-10 Marks)
The skin is the largest organ of the body and serves as the primary physical barrier between the internal environment and the external world. It is the first line of defense in the innate immune system, preventing the entry of pathogens, toxins, and harmful substances. The protective function of skin is achieved through three interconnected mechanisms: physical, chemical, and biological barriers. Together, they provide a robust, multi-layered defense system.
The skin’s physical structure prevents microbial penetration through several features:
- Stratified Squamous Epithelium: The outermost layer (epidermis) is made of multiple layers of keratinized, dead cells that are tightly packed, creating a tough, impermeable shield.
- Keratin: A fibrous protein that provides mechanical strength and water resistance.
- Tight Junctions: Specialized proteins that seal adjacent epithelial cells, preventing pathogens from slipping between cells.
- Continuous Shedding: The outermost layer (stratum corneum) is constantly shed, removing any attached microbes.
- Basement Membrane: A supportive layer that further hinders invasion.
Function: Acts like a “brick wall” to block direct entry of bacteria, fungi, viruses, and parasites.
2. CHEMICAL BARRIER (Biochemical Defense)The skin secretes various substances that create an inhospitable environment for pathogens:
- Acidic pH (pH 4–6): Maintained by lactic acid in sweat and fatty acids in sebum, inhibiting the growth of many bacteria and fungi.
- Antimicrobial Peptides (AMPs): Small proteins such as Defensins (punch holes in microbial membranes) and Cathelicidins (disrupt bacterial cell walls and neutralize viruses).
- Sebum: Oily secretion containing bactericidal fatty acids.
- Sweat: Contains lysozyme (breaks down bacterial cell walls) and dermcidin (a broad-spectrum antimicrobial peptide).
- Salt: High salt concentration in sweat draws water out of microbes via osmosis.
Function: Creates a hostile surface chemistry that kills or inhibits microbial growth.
3. BIOLOGICAL BARRIER (Microbial & Cellular Defense)Living organisms and immune cells on the skin contribute to protection:
- Normal Skin Flora (Commensals): Bacteria like Staphylococcus epidermidis compete with pathogens for space and nutrients and produce their own antimicrobial substances.
- Immune Surveillance Cells: Langerhans Cells (dendritic cells in the epidermis that initiate adaptive immune responses) and Dermal Dendritic Cells & Macrophages (phagocytose invading pathogens).
- Inflammatory Response: Upon injury, localized inflammation increases blood flow and recruits immune cells to the site.
Function: Uses “friendly” microbes and resident immune cells to actively combat invasion.
COORDINATED DEFENSE MECHANISMWhen intact, the skin’s barriers work together seamlessly: The Physical barrier blocks entry, the Chemical barrier kills or weakens pathogens that manage to adhere, and the Biological barrier competes with and alerts the immune system against any breach. This multi-tiered system is highly effective; most infections occur only when the skin is compromised (cuts, burns, ulcers).
CLINICAL SIGNIFICANCEBurns & Wounds: Loss of skin integrity leads to high risk of systemic infections. Dermatological Conditions: Eczema and psoriasis compromise barrier function. Hygiene: Excessive washing can strip away protective oils and disrupt normal flora.
CONCLUSIONThe skin is not merely a passive covering but a dynamic, interactive shield. Its physical robustness, chemical arsenal, and biological defenses collectively form an essential first line of protection, ensuring that the majority of daily microbial challenges are neutralized before they can cause harm.
Skin as a Physical Barrier
2-Mark Questions
Common Model Answer (for 2-mark)
The skin acts as a physical (mechanical) barrier due to its outer epidermal layer, specifically the stratum corneum. This layer consists of dead, keratinized cells (corneocytes) tightly packed with the protein keratin, forming a tough, continuous, and impermeable shield that physically prevents the entry of pathogens into the body.
4–6 Mark Questions
Common Model Answer (for 4–6 marks)
The skin performs its primary physical barrier function through an integrated multi-component system:
1. Keratinized Stratified Squamous Epithelium:The outermost stratum corneum is composed of 15–20 layers of dead, anucleate corneocytes. These cells are filled with keratin filaments and embedded in a filaggrin matrix, creating a dense, chemically inert, and mechanically tough layer that is highly resistant to penetration, abrasion, and enzymatic degradation by most pathogens.
2. Intercellular Lipid Matrix:The spaces between corneocytes are filled with a hydrophobic lipid matrix (composed of ceramides, cholesterol, and free fatty acids). This lipid seal forms continuous multilamellar bilayers that prevent the diffusion of water, water-soluble molecules, and microbes into deeper tissues, thereby waterproofing the barrier.
3. Continuous Desquamation (Shedding):The skin undergoes constant renewal (turnover every ~30 days). The shedding of the outermost stratum corneum cells is an active mechanical cleansing process. It ensures that any microorganisms that manage to adhere to the skin surface are physically removed before they can establish colonization and cause infection.
In essence, the synergy of a resistant keratinized cell layer, a waterproof lipid seal, and constant surface renewal makes the skin a highly effective physical barrier in innate immunity.
8–10 Mark Questions
Common Model Answer (for 8–10 marks)
The skin is the body’s paramount physical barrier, a dynamic and multi-layered structure whose defensive capability arises from specialized anatomical and physiological features. Its role can be detailed under three core structural and functional components:
A. The Keratinized Stratum Corneum: The Primary Impermeable WallStructure: The epidermis, a stratified squamous epithelium, is the key defensive layer. Its outermost zone, the stratum corneum, consists of 15–20 layers of fully differentiated, dead cells called corneocytes. These are flattened, anucleate sacs packed with keratin intermediate filaments cross-linked by proteins like filaggrin.
Mechanism of Action:
- Mechanical Resistance: The dense keratin–filaggrin matrix provides exceptional tensile strength and rigidity, making it resistant to penetration, tearing, and physical stress.
- Biochemical Inertness: This keratinized layer is insoluble and chemically stable, resistant to degradation by many weak acids, alkalis, and bacterial proteases (true “keratinase” enzymes are rare among pathogens).
Structure: Corneocytes are not cemented together but are embedded in a lipid-rich extracellular matrix. This matrix is secreted by keratinocytes via organelles called lamellar bodies and is composed of approximately 50% ceramides, 25% cholesterol, and 10–15% free fatty acids in an organized molar ratio.
Mechanism of Action:
- Hydrophobic Barrier: These lipids arrange into continuous multilamellar sheets (like the layers of an onion) filling the intercellular spaces. This creates a critical hydrophobic (water-repellent) seal that is impermeable to water and water-soluble substances.
- Pathogen Blockade: This seal prevents the passive diffusion of microbes, their toxins, and other hydrophilic noxious agents into the viable epidermis.
- Cohesion: Adjacent corneocytes are linked by specialized structures called corneodesmosomes, which provide mechanical cohesion while allowing for controlled shedding.
Process: The epidermis is a continuously renewing tissue (complete turnover in ~27–30 days). As new keratinocytes are generated in the basal layer, older ones are pushed upward, keratinize, and eventually reach the surface.
Mechanism of Action:
- Controlled Shedding: At the surface, proteolytic enzymes (e.g., kallikreins) cleave the corneodesmosomal links in a regulated process called desquamation. This results in the shedding of the outermost corneocyte layers (approximately one monolayer per day).
- Mechanical Removal of Pathogens: This constant exfoliation acts as an active “cleansing” mechanism. Any microorganisms that have adhered to the skin surface are physically sloughed off before they can multiply, invade, or establish a stable colonization.
The true defensive power lies in the synergy of these components. The keratin layer provides structural integrity, the lipid matrix seals the gaps, and desquamation provides renewal and cleansing. Disruption of any component (e.g., lipid extraction by solvents leading to dry skin, or genetic defects in filaggrin as in atopic dermatitis) compromises the entire barrier, increasing susceptibility to infection, dehydration, and inflammation. Thus, the skin’s physical barrier is not a passive wall but a complex, active, and integrated ecosystem essential for maintaining sterile internal compartments.
Select any Marks Category to view questions and answers